A Glorious Accounting Of Sepsis Overtreatment
Assuredly causing more harm than good, now.
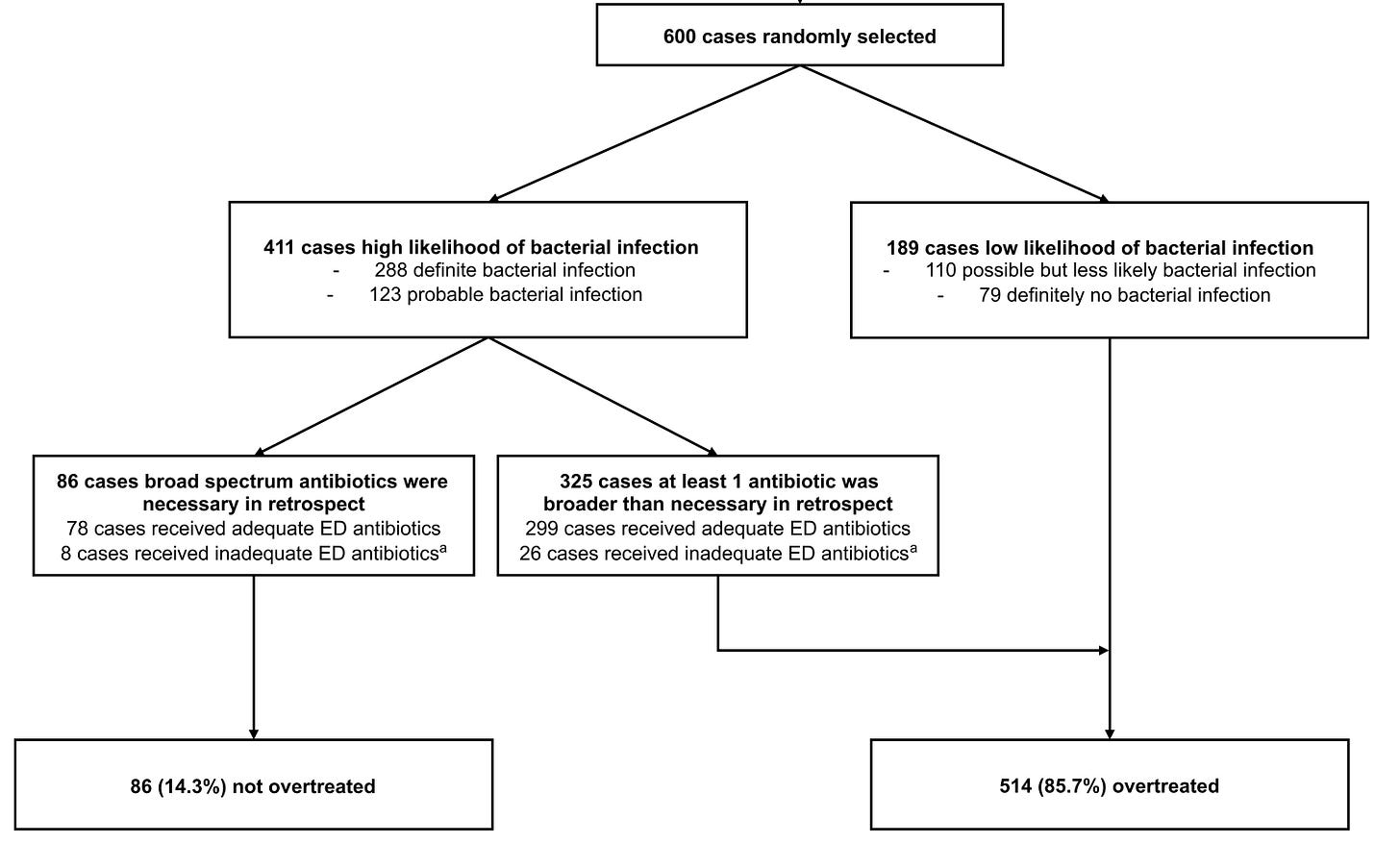
This flowchart pretty much sums it up:
600 patients treated for possible sepsis, focusing on those specifically treated with at least one broad-spectrum antibiotic targeting MRSA and/or an antipseudomonal β-lactam.
As you can see, a preponderance had definite or probable bacterial infection at the time of treatment – but that still left >30% of cases adjudicated to have low or zero likelihood of infectious disease. The net result: 5 in 6 patients in the ED received overly-broad antibiotic coverage.
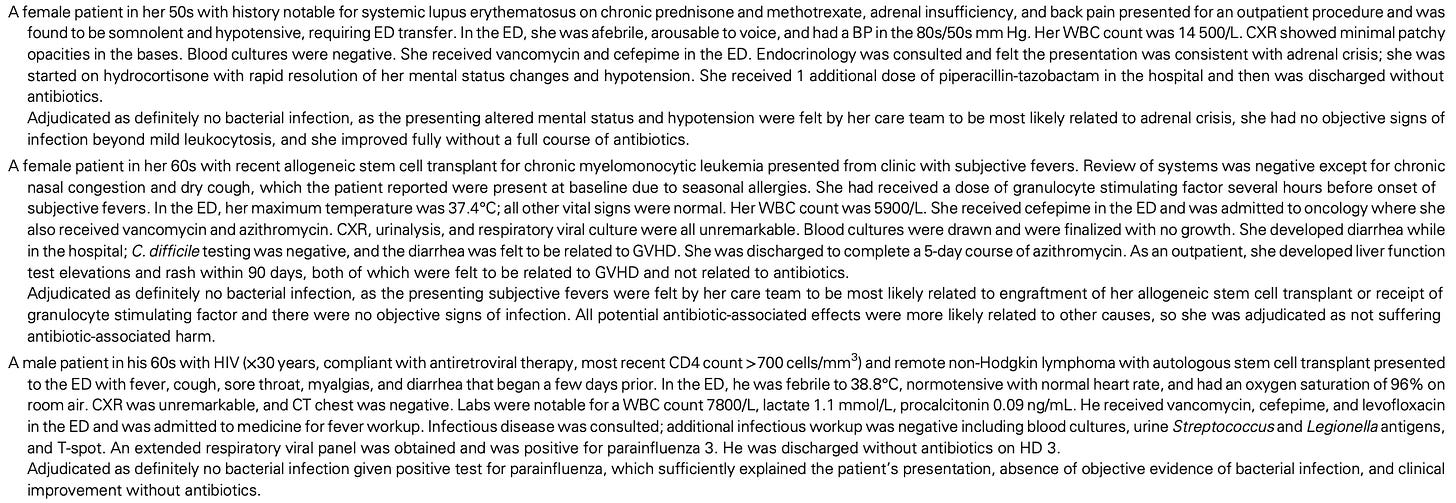
It is fair to say, though, looking at some of their representative cases – the adjudication is a bit harsh. Here are a few of their included examples of “definitely no bacterial infection”:
These cases definitely benefit from the retrospectoscope of having all the information necessary to make the “not an infection” determination!
The authors then go through these cases and note 1 in 5 cases suffered an adverse event attributable to the antibiotics – mostly development of new antibiotic resistance, but a bit of kidney injury and C. difficile infection, as well.
A fair topic for review. Curtailing a decision to treat with any antibiotic is unlikely to garner receptive traction, but critiquing the over-broad choice of antibiotic is very reasonable.