Calcium Pretreatment to Prevent Hypotension
A trial suggesting a better trial is worth doing.
There are many ways to treat atrial fibrillation with rapid ventricular response. One popular method, and the way I originally trained, was chronotropic control with intravenous calcium channel blockers.
Calcium channel blockade affects not only the intrinsic conductivity of the heart, but also peripheral vasoconstriction – as evident by the use of dihydropyridine calcium channel blockers as treatment for hypertension. Whilst diltazem and verapamil have more central activity than peripheral, there is yet some overlap, and a common effect of intravenous rate control can be hypotension.
The idea here: give intravenous pretreatment with calcium, reduce the likelihood of hypotension.
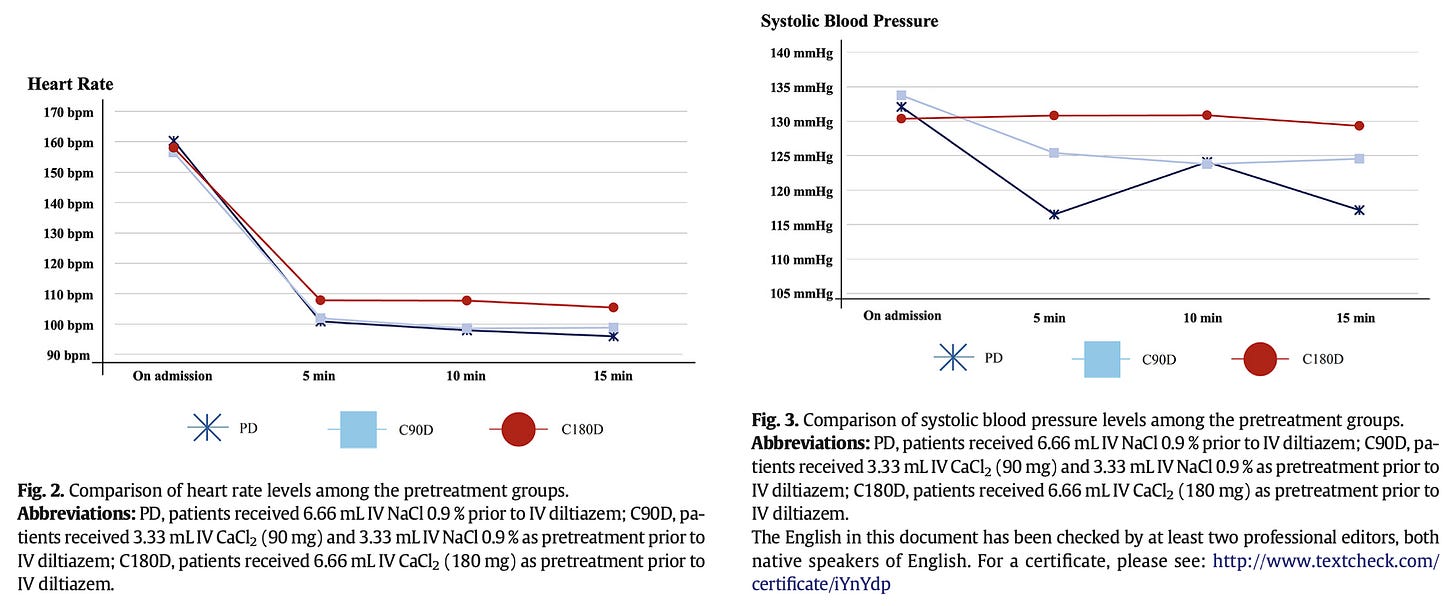
Grossly speaking, in the ~200 patients split into three arms of saline placebo, 90mg of CaCl2 pretreatment, and 180mg of CaCl2 pretreatment, effects on blood pressure were attenuated without apparent negative impact on rate control.
The authors provide the standard deviation for blood pressure in tables in the manuscript, but there’s little documentation here describing the scope of clinically important hypotension – which is already quite infrequent, else CCBs would not be in wide use today.
To build upon these data, it would be ideal if additional prospective trials could be performed with a more “at risk” situation where CCBs are being avoided, or better explore the use and dose range necessary to treat CCB-induced hypotension, after the fact.