More EHR Antibiotic Nannies
It's our own fault, though.
Let’s be serious – antibiotic resistance in U.S. hospitals is a problem, but it’s not so much of a problem everyone admitted with an infection needs to be covered for those organisms.
However, in present culture, you’re vastly more likely to be dinged for under-treatment, rather than over-treatment, and so: we end up plagued by rampant overuse of extended-spectrum antibiotics.
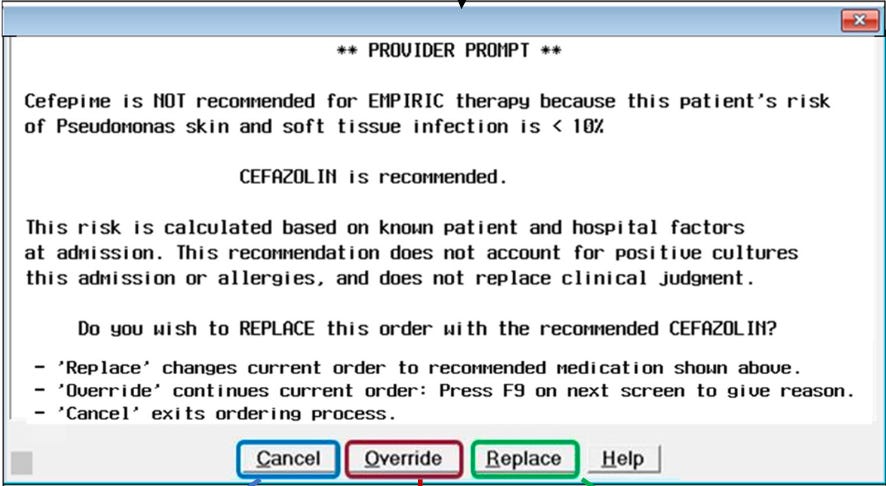
This is a report from a set of HCA hospitals, describing a cluster-randomized implementation of an antibiotic stewardship alert embedded into MEDITECH, as compared with “usual” antibiotic stewardship communication and education. In short, if the EHR was able to determine a patient was at low risk for one of the various MRSA, ESBL, CRE, or Pseudomonas infections, a clinician would see something like this:
In the pre-intervention period (2019), patients admitted for skin and soft tissue infections received extended-spectrum empiric antibiotic therapy in ~56% of admissions. In the post-intervention period (2023), the rate of extended-spectrum antibiotic therapy in hospitals randomized to the EHR alert decreased to 43%, while the other hospitals remained steady. No apparent safety issues could be gleaned from patient outcomes.
There isn’t any information presented here regarding the response to the alerts – frequency of their appearance or behavior change resulting – so the validity of their efforts cannot be fully assessed. However, it is not surprising these alerts had the desired effect considering the fertile ground already sown by the clinical culture of over-treatment.