Perfusion Is Not Just A Number
Lactate is easy to measure, but remember it's just a surrogate.
Measurement of serum lactate has become the cornerstone of sepsis evaluation and treatment, despite its limitations. On the plus side, it’s a simple lab value, easy for chart abstractors to score for compliance with sepsis “quality” goals! On the down side, it’s merely a surrogate for effective end-organ perfusion, for appropriate resuscitation, and there are many potential disease-related confounders.
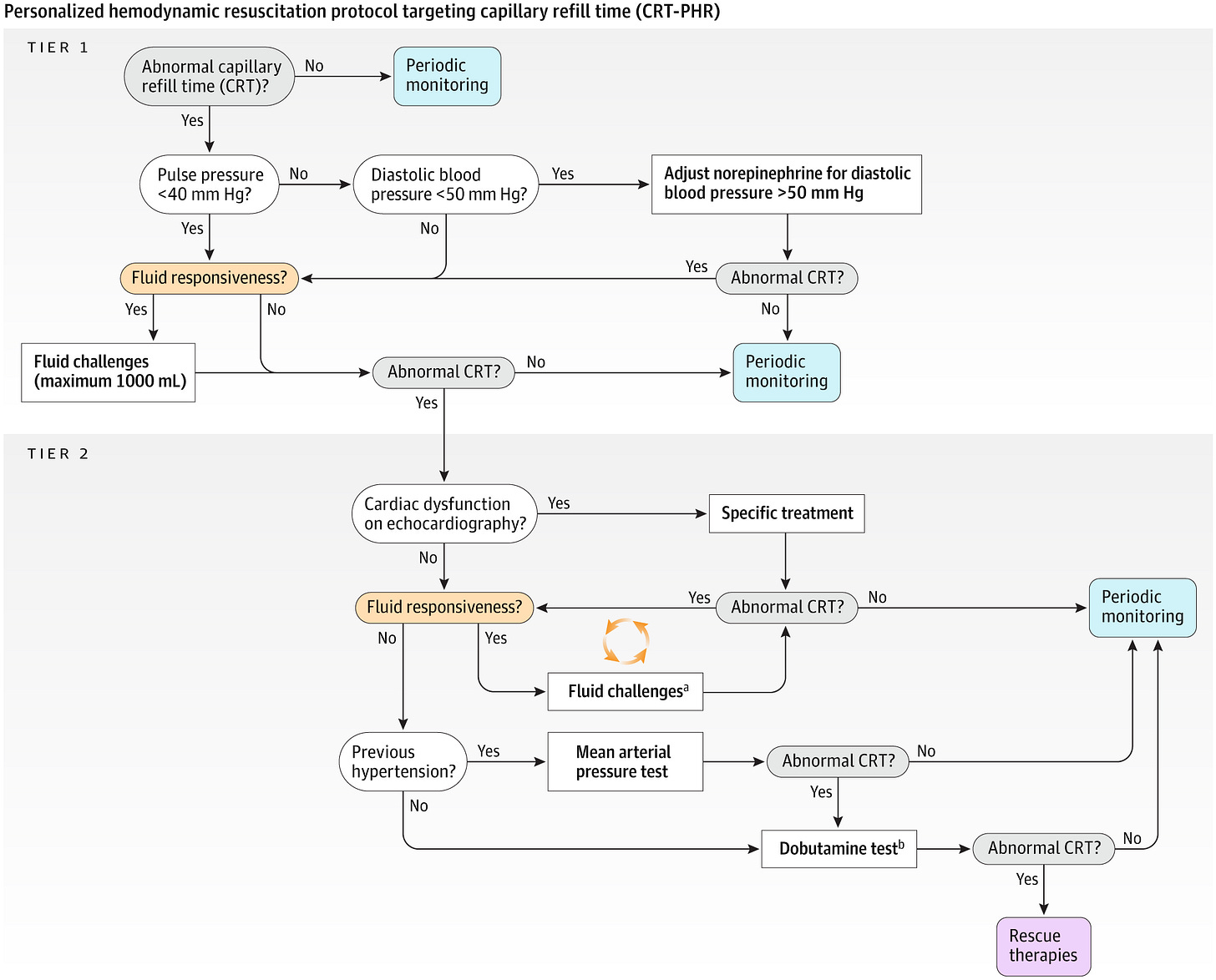
ANDROMEDA-SHOCK 2 eschews the reliance on lactate to further focus on directly measuring the microcirculation based on peripheral capillary refill. It then incorporates this measurement into a robust algorithm of additional measures of fluid responsiveness, left-ventricular dysfunction, etc.:
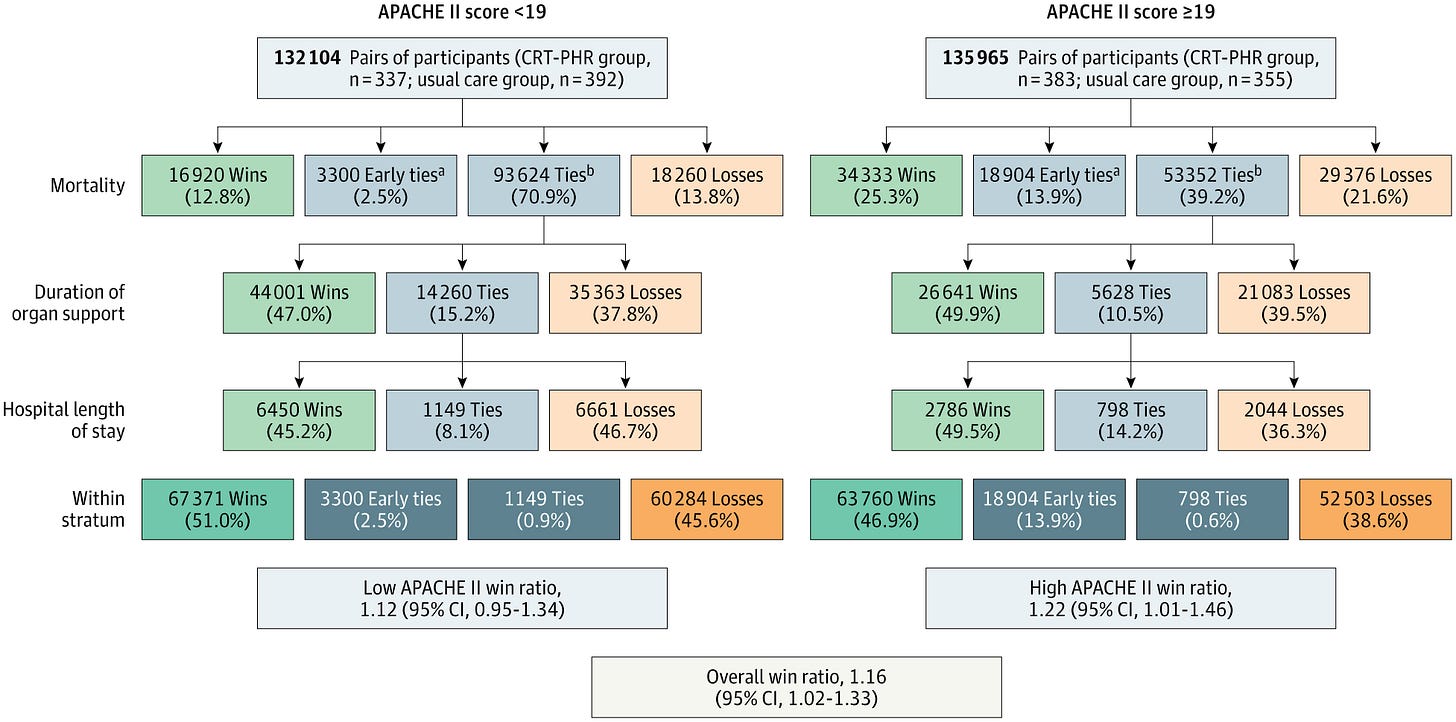
The result of their protocol? Additional “wins” for their composite endpoint, as you can see below:
There is a lot to unpack, both from a superficial sense and in an extensive supplementary appendix. For example, patients were excluded if their skin color were too dark to accurately assess capillary refill – a very problematic criterion in certain practice settings. Then, is “usual care” inferior because of its reliance on traditional measures of sepsis resuscitation, or because it lacks the robust protocol for fluid responsiveness and LVEF evaluation? This hearkens back to early goal-directed therapy for sepsis where it was difficult to ascertain the important piece out of the entire bundle of care delivered.
A little “light” weekend reading!