Reversing "Immune Paralysis" in Sepsis
A glimpse of the far future.
As opposed to what is called “sepsis” in every over-reacting emergency department in the U.S., there is True Sepsis – the dysregulated immune response to infection. But, peeking under the hood of True Sepsis, there is a heterogeneous mix of phenotypes of dysregulation. The implication of this being, if treatment were tailored to the type of dysregulation, outcomes might be further improved beyond those offered by the blunt tools of antibiotics and non-specific organ-support.
This “ImmunoSep” study (not to be confused with the IntelliSep product) offers a glimpse of that potential future. Here, these authors describe a potential phenotype of immune dysregulation in the critically unwell manifesting either a hyper-inflammatory macrophage activation (ferritin >4420 ng/mL) or immune paralysis (ferritin <4420 ng/mL and <5000 human leukocyte antigen DR receptors on CD45/CD14 monocytes).
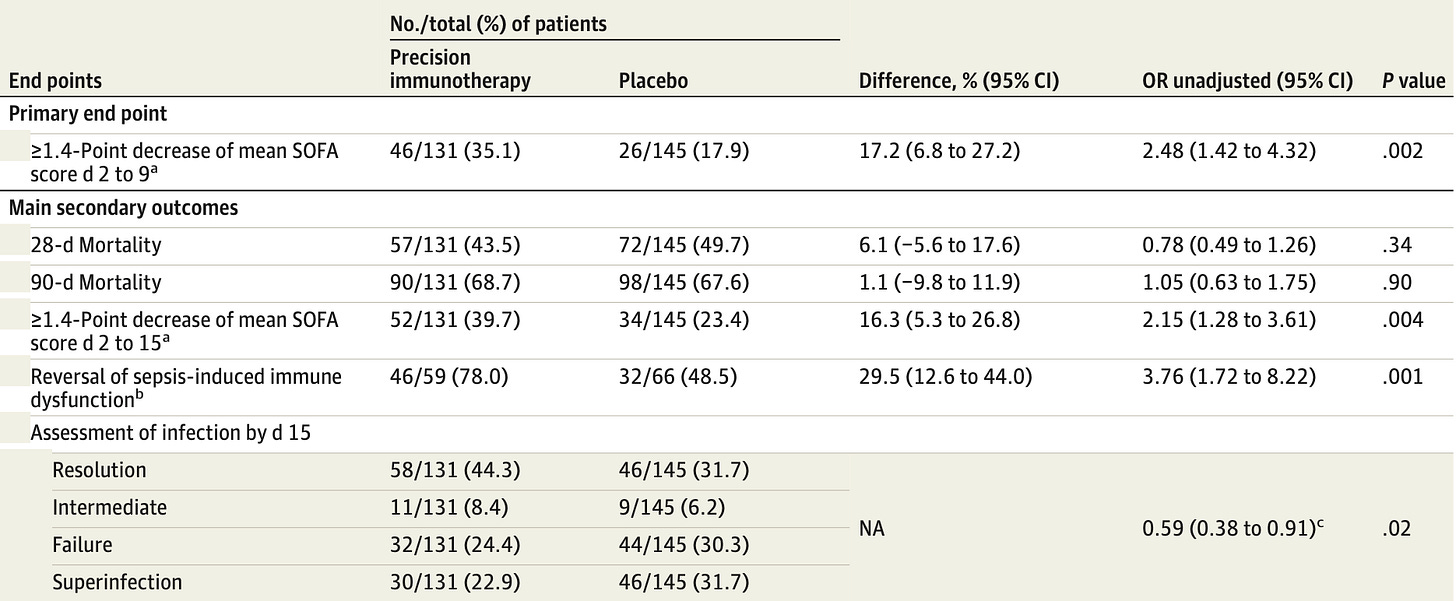
Patients were only eligible for inclusion for lower-respiratory tract infections, the vast majority of which were mechanically ventilated, and most exhibited the immune paralysis subtype of this phenotype. These patients were then treated with anakinra (IL-1 antagonist) or placebo. Surrogate and short term outcomes were modestly improved, with the improvement outweighing the adverse effects from treatment:
Is this particular treatment ready for prime time? Hardly. These are promising results, but rely upon the surrogate SOFA score rather robust patient-oriented outcomes. If these findings reflected the ideal targeted therapy for a validated phenotype, there ought to be a stronger relationship between the two.
However, I suspect this is a valid path forward to an era where treating infection is more sophisticated than broad-spectrum antibiotics, systemic steroids, and other non-targeted therapies.