Should You Take Antihypertensives At Bedtime?
"Should you" vs. "can you".
Whenever a medication is administered, there is naturally an uptick in serum concentration as the medication is absorbed. Depending on the medication, this can result in an increased clinical effect. For some anti-hypertensives, that increased clinical effect is a resultant drop in blood pressure – and this can be good (health protection) or bad (adverse events from over-correction).
One interesting observation has been made in patients taking their once-daily blood pressure medications before bedtime. The effect of blood pressure lowering appears to be potentiated overnight, as compared to the effect on daytime blood pressure after a dose taken in the morning. This leads to better average 24-hour blood pressure control, overall, and a couple studies have associated this better control with improved cardiovascular health.
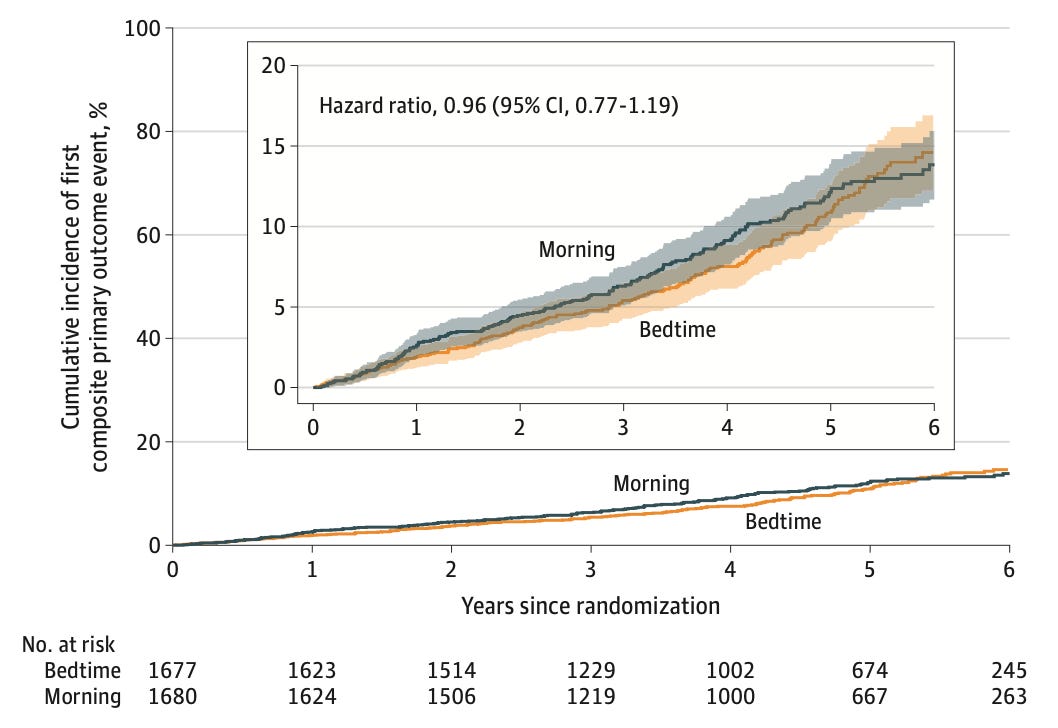
This week, we have BEDMED, another trial, and one performed in a Canadian population slightly more comorbid than those in the previous trials. Over the six-year trial period, the authors found no difference in the primary outcome, a composite of death and major cardiovascular events:
So, no, taking medication at bedtime may not be as magical as potentially considered. There were truly no reliable signals of difference between each arm, whether in the primary outcomes of cardiovascular events, nor the safety outcomes of falls and lightheadedness. However, in a small group of ~300 patients agreeing to undergo 24-hour blood pressure measurements, these authors did confirm the prior observation the bedtime antihypertensive cohort did spend a greater amount of time in the recommended blood pressure range.
There were differences in this trial than the prior ones – one of the most notable being there were large numbers of this trial cohort taking twice-daily antihypertensive medications. It may be the effects of bedtime antihypertensive administration are diluted by the presence of so many twice-daily agents. There were also, overall, very few events, leading to wide confidence intervals – but a large beneficial effect is likely excluded.
I am uncertain which is more desirable: improved control in the night, leading to fewer 2AM emergency department visits for high blood pressure, or correspondingly higher blood pressure during the day, leading to more referrals to the ED by primary care offices?