The OPTION For Tenecteplase Out to 24 Hours
In theory.
I’ve been on the “tissue not time” paradigm for a least a decade:
This has been demonstrated repeatedly over the past 15-odd years. Tissue-based salvage is the foundation for endovascular therapy in large-vessel occlusion, as well as ideas behind using MRI-based imaging parameters for so-called “wake-up stroke”.
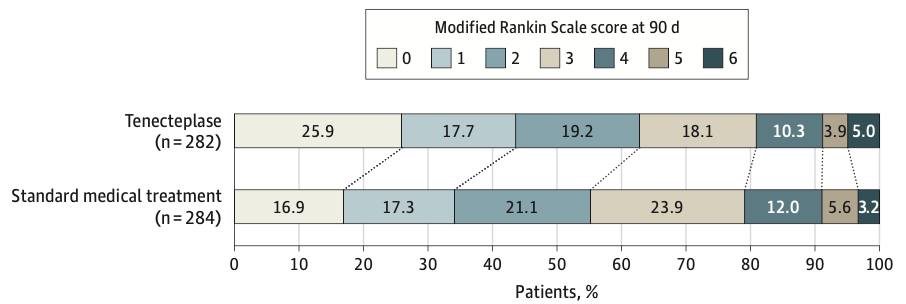
This study is the most recent progression of this concept, using tenecteplase between 4.5 and 24 hours for patients with non-LVO, NIHSS < 26, and sufficient perfusion mismatch on CT perfusion imaging. Here’s your winner:
As with most stroke interventions, there is a risk of intracranial bleeding resulting in an excess of death.
In theory, I still generally agree with the principles behind this study. Viable tissue paired with successful reperfusion is a straightforward key for success. However, reperfusion at 24 hours was terrible, only 37.7% in the tenecteplase cohort versus 28.8% with standard therapy. It strains face validity for the magnitude of the primary outcome to hew so closely to one of the minimum physiologic requirements for clinical response.
And, then, there are two other issues tilting the playing field towards tenecteplase:
94.0% of the tenecteplase group were mRS 0 at enrollment, as compared with 89.8% of the standard medical cohort. A more functional group at entry has a built-in advantage for the primary outcome.
Occlusions in the M2 segment were dominant (>50% of the vascular territory of the MCA) in 19 patients in the standard medical cohort and only 8 in the tenecteplase cohort – whereas an excess of codominant and non-dominant M2 segments enriched the tenecteplase cohort. An additional 3 patients were in the standard medical cohort had M1 occlusions. These will all negatively influence outcomes in the standard medical cohort, regardless of the initial imaging-based appearance.
These idiosyncrasies will be swept under the rug by the prevailing stroke industrial complex, of course, and we’ll simply see more indication creep for thrombolysis (and, naturally, no adoption of negative tissue-based evaluation for patients within the time window).