The Precarious Race of "Point-of-Care Troponin"
It's frequently a zero-sum game, anyway.
This little article we just podcasted for Annals of Emergency Medicine reminded me how focus on this topic usually misses the forest for the trees.
The basic gist: if you have a point-of-care troponin assay, you can get results back faster than sending the same sample to the lab. If you get your troponin assay result back sooner, you can get your patient discharged faster. The emergency medicine/cardiology literature, then (frequently sponsored by the manufacturers of the diagnostics), focuses on this improvement in time-to-disposition.
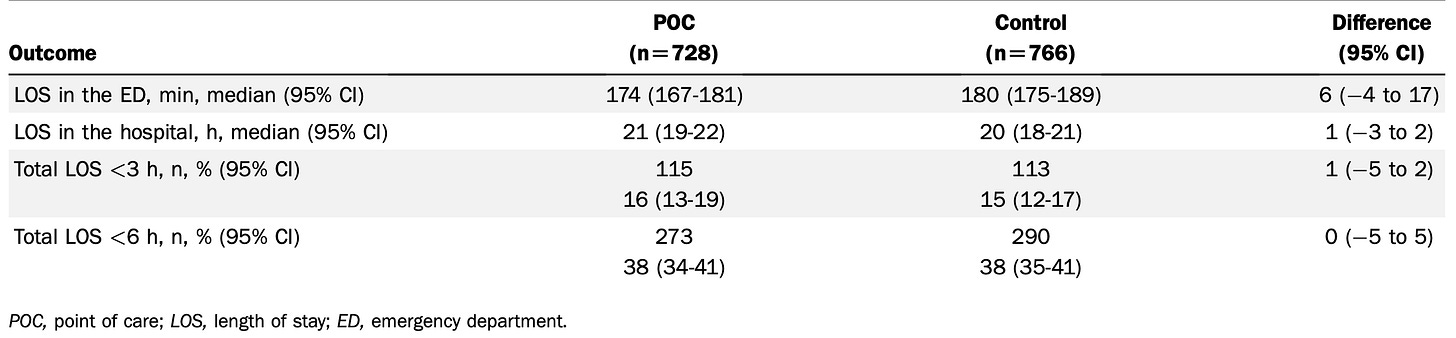
In the article Rory and I discussed, amusingly, there wasn’t much difference:
Troponin results were available 30 minutes faster in the point-of-care arm, but LOS was improved by 6 minutes, and proportions with early discharge were unchanged. This is, in part, due to problematic study design and inefficient surrounding processes. We in Christchurch have been using POC troponin for quite some time, and before-and-after observations show improvements in time-to-disposition.
But, what all these studies miss is that time-to-disposition for the patients with chest pain ignores the zero-sum nature of an overburdened emergency department. Yes, perhaps that one patient is eligible to be turned around sooner. However, following up on the result for that patient simply re-orders the disposition queue, pushing other patients back a few minutes each, and the cumulative dwell time for all patients remains the same.
Now, if you have a department that is firing on all cylinders and there is latent emergency department clinician time where responding to an early troponin result does not impact the care of other patient, you have a win. But, the point still stands – the improvements seen for patients with chest pain cannot reliably be generalized to an improvement in efficiency for the entire ED.